
Access to care for back pain, food insecurity, and abnormal vaginal bleeding. Overcoming the barriers to care posed by the high costs of transportation to clinic and missing work. Care delivered in a way that respects both dignity and privacy. Those are some of the top health care priorities identified by women in rural Rwanda in a study published recently in the International Journal of Gynecology and Obstetrics.
The mixed-methods study was conducted in two phases by researchers from the Center for Integration Science in Global Health Equity based at Brigham and Women’s Hospital (CIS) and Partners In Health Rwanda/Inshuti Mu Buzima (PIH/IMB).
In the first phase, the researchers conducted semi-structured interviews with 17 women of child-bearing age (20-49) in three rural districts. The interviews explored what the women considered to be their highest priority health concerns (not including childbirth and oncology), as well as how they felt about their previous experiences accessing health care and their preferences for healthcare delivery. In the second phase, 150 other women from the same catchment areas responded to a quantitative survey designed to explore healthcare priorities and preferences based on qualitative data from the interviews.
Priority health concerns identified
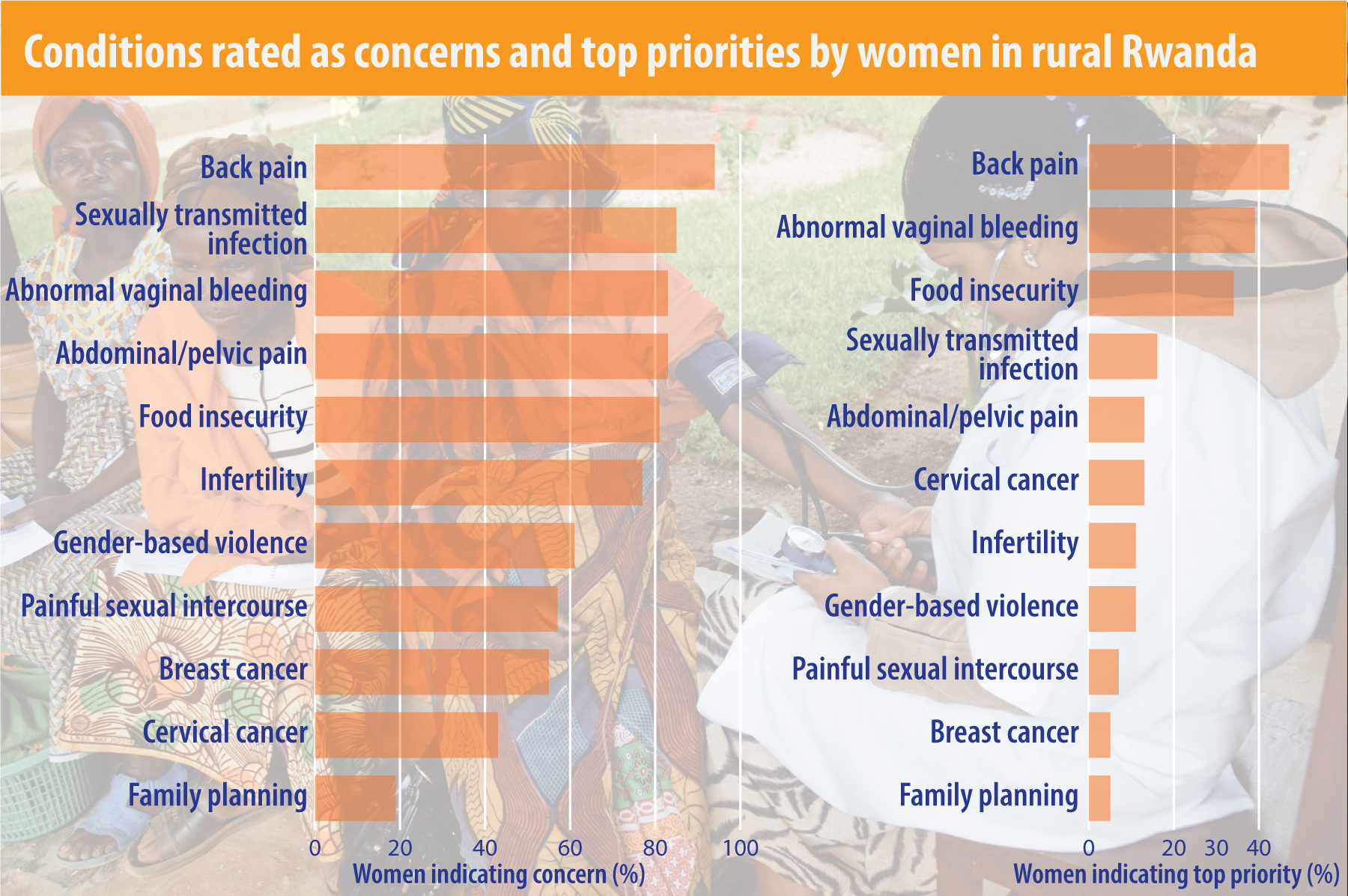 In the interview phase, women cited 11 communicable and noncommunicable health conditions as their top health priorities. More than half of the women who participated in the survey (55%-94%) then confirmed that nine of these 11 conditions – back pain, sexually transmitted infections, abnormal vaginal bleeding, abdominal/pelvic pain, food insecurity, infertility, gender-based violence, painful sexual intercourse, and breast cancer – ranked as major concerns among women in their communities.
In the interview phase, women cited 11 communicable and noncommunicable health conditions as their top health priorities. More than half of the women who participated in the survey (55%-94%) then confirmed that nine of these 11 conditions – back pain, sexually transmitted infections, abnormal vaginal bleeding, abdominal/pelvic pain, food insecurity, infertility, gender-based violence, painful sexual intercourse, and breast cancer – ranked as major concerns among women in their communities.
When the women were asked to pick the two most important conditions of concern in their communities, back pain, vaginal bleeding, and food insecurity emerged as top priorities, selected by more than one-third of participants.
“We just went with really open-ended questions,” commented Alma Adler, CIS director of research and lead author of the study. “What are you concerned about? How do you feel about the care you have received and how it was delivered?”
Addressing barriers to care and dignified care delivery
Women generally reported positive experiences while accessing care. But they identified transportation costs and inability to miss work as important barriers to care that reduced accessibility. And they made it very clear that they believe care should be provided in ways that respect their privacy and dignity.
Participants affirmed unanimously that exams should be conducted in private rooms or behind curtains and indicated a distinct preference for having breast and internal exams conducted by female providers. Nearly all of the women (94%) felt comfortable with having breast and internal exams with female providers. But more than a third of participants (37 percent) indicated they do not feel comfortable having a man examine them internally – matching almost exactly the 36 percent who said they would like to bring a companion to an exam.
In addition, the women expressed a strong desire for more control over their care, including being fully informed about diagnoses, medications, and procedures and having a voice in healthcare decisions.
“If I get pregnant again, I will have to ask the doctors why they use the C-section surgery, because they didn’t give me any explanation.”
– Woman patient interviewed in rural Rwanda
Participants in the survey were all but unanimous (95-100%) in agreeing that it is important to have procedures described before they are done, to have diagnoses explained before they leave medical appointments, and to know what medications they are taking. More than two-thirds (69%) said they want to be able to choose what treatment is available.
“These findings are very important and real,” Adler said. “The research starts conversations that people should have had decades ago.”
Lessons for service delivery design
The findings will inform ongoing work at both the Center for Integration Science and PIH/IMB to improve quality and access to care for women living in poor, rural areas.
The Center for Integration Science is working with partners in the NCDI Poverty Network to develop models for a women’s health outpatient clinic at district hospitals to provide advanced gynecologic and breast health.
Similarly PIH/IMB is supporting the Rwanda Ministry of Health’s efforts to expand breast and cervical cancer screening as part of a broader panel of services intended to meet women’s expressed healthcare priorities and preferences.
“Findings from this research and continued engagement with women living in these poor, rural areas will help ensure that these integrated packages of interventions address women’s priority health concerns, help them overcome barriers that might limit access to that care, and deliver the care in ways that allow them to feel respected and comfortable,” Adler concluded.
Or as the conclusion of the article puts it: “The reported end-user health concerns, barriers to care and diminished control over their care unmet needs, point to a requirement to evolve our health systems around seeker-tailored needs and design urgent interventions that optimize access whilst promoting women’s dignified care.”
